Wow!!!! I am humbled by the overwhelming response I received in response to yesterday’s post, Lymphedema and How It Has Changed My Life. So many of you have shared your experience with lymphedema, whether you got it as a result of breast cancer treatment, another surgery or trauma or as a hereditary condition. This has made me believe, even more strongly than before that we need more research, education and awareness for this disease. What an incredible community we are creating when we share our experience.
Today, March 6, is officially World Lymphedema Day, which makes me even more thrilled to introduce to you, Cynthia Shechter of Schechter Care. Cynthia is an OT specializing in breast cancer and lymphedema rehabilitation. She is not only the OT that has helped me manage what I thought was a condition that would only get worse with time and could not be helped, she has become a dear friend. She is also a fierce advocate for the disease.
If you have any additional questions for Cynthia, I hope you will leave it in the comments section or feel free to email me (see my contact information above) if you would like your question to remain private. And continue to share your experiences. Knowledge is power.
It is my honor and pleasure to introduce Cynthia to you all.

Photo of Cynthia Shechter, taken from shechtercare.com
What is your full name and what do you do? Cynthia J. Shechter and I am an occupational therapist specializing in Breast Cancer and Lymphedema Rehabilitation
What is your training and are you licensed? ? I received my bachelors degree in clinical sociology from Ithaca College, my Masters In Occupational Therapy from NYU and have trained and been certified by The Klose School for lymphatic education. http://klosetraining.com. I also trained with the Academy of Lymphatic Studies and with Linda Miller, a true mentor in the field. I am licensed to practice in New York and New Jersey.
How long have you been practicing? I have been an OT for 14 years and have specialized in this field for over 10.
There are so many specialties of physical therapy. I am an OT, not a PT, although the lines definitely blur, with this particular specialty Why did you choose lymphedema and breast cancer as your area of focus? It was really by chance. I thought that I wanted to be a hand therapist and while working in hands I identified that I could help my patients more effectively if I could better control their swelling. Since lymphatic drainage is only touched on in graduate school, I decided to go get trained so that I could help improve orthopedic surgical outcomes by getting rid of swelling rapidly, increasing range of motion and functional hand use. In my first few training courses I learned a lot about lymphedema, breast cancer, treatment, etc. I extended my clinical focus to include breast cancer and lymphedema, and found my true passion in doing so. I realized that I could do so much more for this underserved population of patients by advocating for them, helping them through the healthcare maze, using my psychosocial training, and by thinking outside the box in terms of treatment. The more I treated breast cancer and lymphedema, the less I wanted to treat hands, and here I am today, evolved into the therapist I always hoped to be.
Is everyone who gets a mastectomy or lumpectomy at risk for getting lymphedema? Unfortunately, yes.
How long does it take to get lymphedema after a mastectomy? Researchers say that lymphedema typically occurs in the first 2 years post op, but the risk is lifelong. I have many patients whose swelling didn’t begin for 20 years post.
When it comes to breast cancer, is lymphedema a woman’s issue or can it happen to men as well? Lymphedema does not sexually discriminate, anyone can get it regardless of gender.
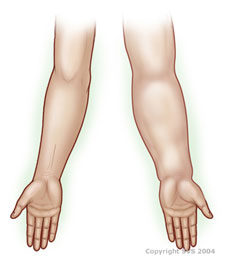
What signs should women who have had a mastectomy look for to detect lymphedema? Lymphedema can be subtle at first, and I believe strongly that EVERYONE who has had surgery for breast cancer should receive rehabilitation, even if only or a short period of time. Here are some what to look for from the ACS:
“Signs and symptoms of lymphedema can include:
Swelling in the breast, chest, shoulder, arm, or hand
Part of your body feeling full or heavy
Skin changing texture, feeling tight or hard, or looking red
New aching, tingling, or other discomfort in the area
Less movement or flexibility in nearby joints, such as your shoulder, hand, or wrist
Trouble fitting your arm into jacket or shirt sleeves
Your bra not fitting as well as it used to
Your ring, watch, and/or bracelet feeling tight, and you haven’t gained weight
Early on, the skin usually stays soft, and raising your affected arm might relieve the swelling. But over time, the swollen area may become hot and red and the skin hard and stiff.
If you’ve had any type of breast surgery, lymph nodes removed, or radiation treatment, look at your upper body in front of a mirror. Compare both sides of your body and look for changes in size, shape, or skin color. Get to know your body and what’s normal for you. This way you can spot changes and get treatment right away.”
How is lymphedema typically treated? Lymphedema is traditionally treated with Complete Decongestive Therapy, CDT.This link from breast anger.org gives a good description of each component of CDT http://www.breastcancer.org/treatment/lymphedema/treatments/cdt
You tend to “bend the rules” when it comes to standard care of lymphedema. Can you speak to your philosophy of lymphedema care? My overall philosophy is to assist patients in living WITH lymphedema, not FOR it. it Is important for a clinician to listen to what each individual says regarding their care and tolerance of bandages, including time spent wrapping and being wrapped. Nothing in this world is black and white, we all exist in the gray areas, lymphedema is no exception. I think that it is important to treat patients as people, not as a condition. Although CDT is a proven treatment, I think it is so important to modify recommendations to work with a patients lifestyle, and, not everyone responds to traditional therapy well. I believe that it is important to use my training as a guide, but not as a definite set of rules. This helps me respond to the progress each patient is making. I modify my manual therapy, by changing the amount of pressure that I use on the tissue, which helps decrease the amount of tissue fibrosis that individuals have. I change whether or not I use a compression pump, foam for bandaging, sleeves are often not tolerated, and bandaging techniques can vary. When treatment is not modified, patients are often nervous, depressed, and angry about their condition. I find that my patients are more in control of their condition, and less afraid to live their lives.
Is lymphedema reversible? Please explain. If swelling is identified early, it can be reversed.
What is your opinion of how doctors are educated about lymphedema? Unfortunately, doctors do not receive much training about the lymphatic system in general and although there is a lot more awareness of the condition, patients are just not educated early.
How can doctors better educate their patients about the risks of lymphedema? Doctors should refer their patients to a clinical specialist in rehabilitation after breast cancer surgery. I think doctors have to understand that lymphedema – this is an unfortunate side effect that will affect some of their patients. That early intervention is important, that prevention is possible; that it is insane to tell someone that they cannot lift more than five or ten pounds forever, that all patients who undergo total hip replacement or rotator cuff surgery receive rehabilitation therapy without a second thought, and breast cancer surgery should follow the same protocol. That we all deserve a chance to move freely and pain free after mastectomy; that we can work to decrease a patients risk of developing lymphedema; that rehabilitation therapists are an integral part of recovery from breast cancer.
Can lymphedema be dangerous? Yes. The lymphatics are responsible for filtering out impurities in the body. When they are not functioning properly, patients are at risk for developing cellulitis, lymphangitis and other serious systemic infections.
What are the physical and psychological effects of lymphedema? I treat my patients based on their lifestyles, activities, needs, and a realistic plan for them to be able to manage their swelling once discharged from active treatment. When patients come to me, they tend to feel helpless with the condition. Lymphedema can be unpredictable, and can flare up at times you would never expect. Also, especially for those individuals with leg swelling, this condition can and does limit basic things that we all take for granted, like what pants we wear, or what shoes we wear to the office. Depending on the severity of ones swelling, and despite use of compression garments, swelling can worsen simple because an individual is standing or sitting for too long. Patients with lymphedema may experience pain caused by the swelling and pressure on nerves, loss of muscle tone and function, range of motion limitations, and/or scar tissue formation. It is important to note, however, that not all individuals with lymphedema have pain. Each patient is treated like an individual. Once a patient is evaluated, I continue to re-assess visit to visit to ensure that what I am doing is actually helping. There are times where I use a vaso-pneumatic pump, teach self bandaging, compression garment use, self massage, brushing, etc. I think the most important thing for me to do as a clinician is LISTEN to my patients’ feedback and modify what I do so that I can help them more affectively. Effective lymphedema treatment is dependent on the patient/clinician relationship. Here is an article written about the overwhelming affects of lymphedema on psychosocial health and lymphedema. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4153404/ I’m not a a mental health practitioner, but often I find that my patients are more distraught about their lymphedema than they are about having had a mastectomy or even breast cancer. I believe that this I correlated to the fact that they are educated about their breast cancer, they were educated about their reconstructive surgery and made an educated decision regarding their treatment and surgical plan. Unfortunately, especially with the finite set of rules and lack of flexibility in the way lymphedema is treated, this is the one area that patients truly have no sense of control. It is overwhelming. What I hope is that in changing the way that lymphedema is treated, I can give people back their sense of control, and help them find options and a management regimen that will work within their lifestyle. Patients with lymphedema tell me that this insidious disease is a constant reminder of their cancer, and affects self esteem in ways that no one could imagine. Lymphedema and the rules associated with the diagnosis of lymphedema can create an incredible fear to go on with life, lift your children, climb a mountain, run a marathon, or simply carry your groceries.
If you could give women one piece of advice about lymphedema, what would it be? Don’t give up on managing your lymphedema. Find a therapist who can listen to you and respond to your individual needs.
If you could give doctors one piece of advice about lymphedema, what would it be? Go for therapy post operatively to help prevent it and if you have swelling already, please don’t be defeated by this insidious condition. It’s a matter of finding the right care for you.
What should a woman/man do if she suspects she might have lymphedema? Find a therapist and begin therapy early.
If a woman does not live in an area where there are many resources for dealing with lymphedema, like here in NYC, what should she do? Go to the national lymphedema network website to find care.
What is the future of lymphedema treatment? I don’t know, but I am excited to find out!
You can contact Shechter Care directly at
shechtercare.com
18 E 48th St. ste. #801
New York, New York 10017
212-421-1969